Macular Degeneration
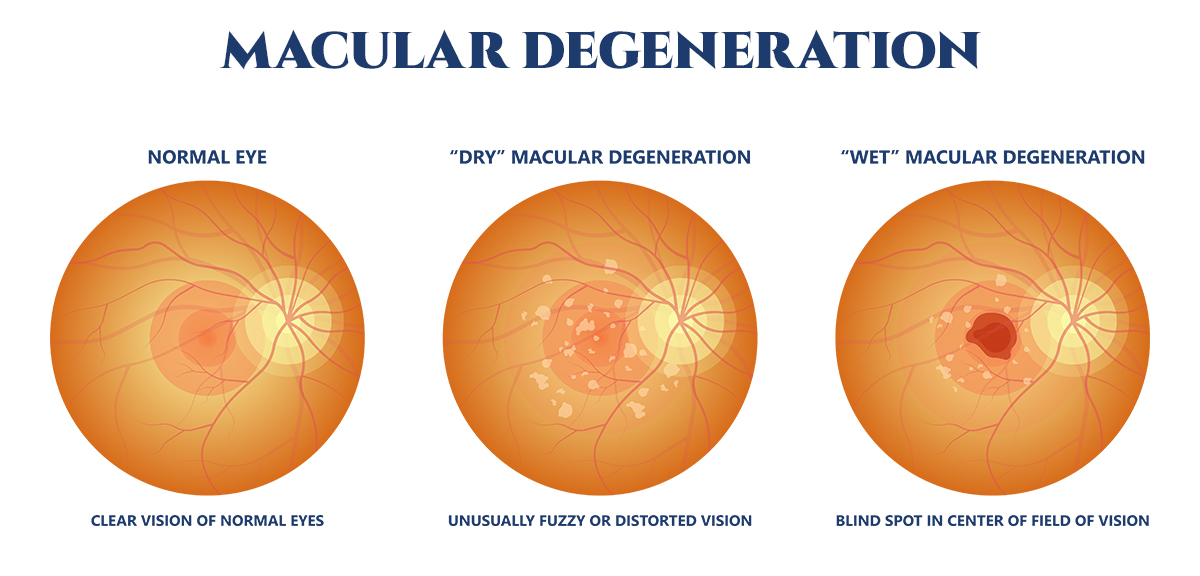
Macular degeneration, although primarily an age-related disorder, can also manifest in younger individuals and has been linked to a variety of indicators such as hereditary factors, nutritional deficiencies, head injury, and diabetes. There are two classifications of AMD – dry or non-exudative AMD (also called atrophic AMD) and wet or exudative AMD (also called neovascular). Scientists are actively investigating the conditions that may lead to cases of early-onset macular degeneration.
Age-related macular degeneration (AMD) can lead to a progressive deterioration of your sight, as the macula – the part of the retina responsible for sharp vision and color perception – becomes damaged. By recognizing the early signs, you may be able to take preventive measures that help slow down the progression. With AMD, there is a loss of central vision and you may not be able to see fine details – but peripheral (side) vision may remain normal. AMD is a leading cause of vision loss for those aged 50 or older.
Dry Age-related Macular Degeneration
Dry age-related macular degeneration (dry AMD) is a chronic eye disease that affects the macula, the central part of the retina responsible for sharp, detailed vision.
For those experiencing dry AMD, the macula gradually thins and breaks down over time, leading to the loss of vision in the central visual field. Small, yellowish deposits called drusen may also accumulate in the macula, interfering with normal vision. Dry AMD progresses slowly and may not cause noticeable symptoms in its early stages, but as the disease advances, vision loss can become more pronounced and may affect daily activities such as reading, driving, or recognizing faces.
Dry AMD Diagnosis
Early diagnosis is key for treating dry AMD. Regular eye exams, including dilated examinations and advanced imaging tests like OCT, can help to reveal any signs of the condition before vision loss occurs. By taking advantage of these preventive measures you can make efforts to protect your sight.
Treatment for Dry AMD
There is currently no cure for dry AMD, but there are some treatments that may help slow down the progression of the disease and preserve vision. These treatments include taking AREDS2 vitamins (available over the counter) twice a day, making lifestyle changes such as quitting smoking or exercising regularly, and undergoing regular eye exams to monitor the progression of the disease.
In advanced cases of dry AMD, certain types of low vision aids may help improve vision and quality of life. Low vision aids can include magnifying glasses, telescopes, and other specialized devices that can help magnify images and make them easier to see.
Wet Age-related Macular Degeneration
Wet age-related macular degeneration (wet AMD) is a chronic eye disease that affects the macula, the central part of the retina responsible for sharp, detailed vision. Wet AMD is a more advanced and severe form of age-related macular degeneration.
For patients that have wet AMD – abnormal blood vessels grow beneath the retina and leak blood and fluid – leading to swelling and damage to the macula. This can cause vision loss, distortion, and blind spots in the central visual field. The early stages of wet AMD may not cause noticeable symptoms, but as the disease progresses, vision loss can become severe and rapid. If left untreated, this condition can cause permanent vision loss and blindness.
Wet AMD Diagnosis
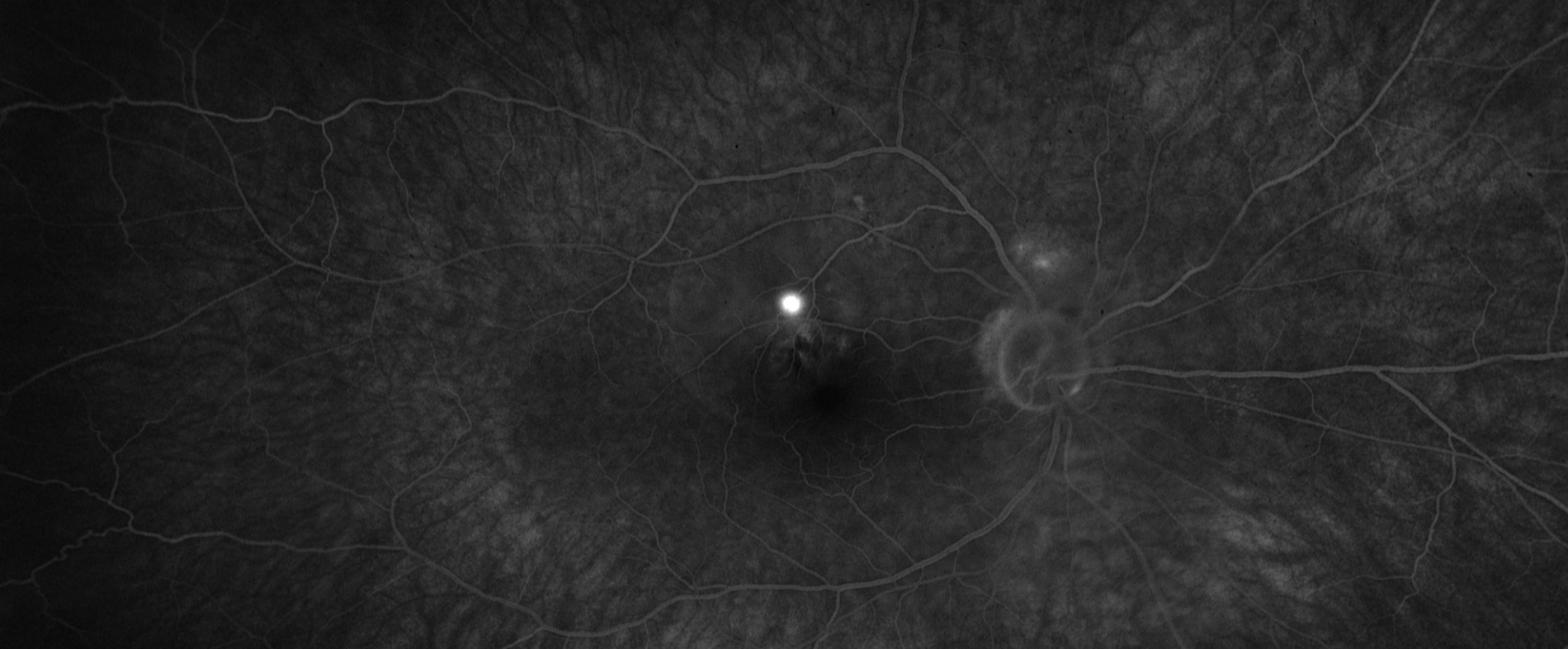
Your regular ophthalmologist or your retina specialist may diagnose your condition by reviewing your medical records and family history, as well as conducting a complete eye exam. A thorough eye exam, including a dilated eye exam and imaging tests such as optical coherence tomography (OCT) can help detect wet AMD in its early stages – allowing for early intervention and treatment to prevent vision loss.
Treatment for Wet AMD
Treatment for wet AMD may include injection of medications called anti-VEGF (vascular endothelial growth factor) drugs, which can help block the abnormal blood vessels and reduce the leakage of fluid and blood in the retina. These medications have had a miraculous effect on the prognosis of wet-AMD. Other less common treatments may include laser therapy or photodynamic therapy (PDT), which use lasers and special dyes to destroy abnormal blood vessels in the retina.
Geographic Atrophy
Geographic atrophy (GA) is a type of advanced dry age-related macular degeneration (AMD) that results in the progressive loss of the cells in the macula, the central part of the retina responsible for sharp, detailed vision. GA is characterized by the appearance of a patch of dead cells in the macula that gradually expands and spreads over time.
As the dead cells in the macula increase, vision loss may become more severe and pronounced, and can eventually lead to legal blindness. GA is a slow and progressive disease that can take several years to develop, and is often bilateral, meaning it affects both eyes.
Geographic Atrophy Diagnosis
As a form of macular degeneration that has progressed beyond AMD, it is diagnosed by an eye doctor during a dilated exam and/or with retinal imaging. Unfortunately, geographic atrophy progression is unrelenting and cannot be reversed – it can lead to a gradual loss of vision as lesion growth steadily continues.
Treatment for Geographic Atrophy
Currently, there is no cure for GA, and treatments are limited to managing the symptoms of the disease. Some treatments that may help slow down the progression of GA include taking antioxidant supplements, healthy food choices, making lifestyle changes such as quitting smoking or exercising regularly, as well as undergoing regular eye exams to monitor the progression of the disease.
In February of 2023, the FDA approved SYFOVRE™ (pegcetacoplan injection), the first ever intravitreal injection to treat GA. This treatment has shown promise in improving outcomes in this previously untreatable disease as it is meant to help regulate an overactivated part of the immune system in the patient’s eye, because this overactivation can contribute to the progression of GA.
While GA cannot be cured, and any damage from lesion growth cannot be reversed, SCRI is currently offering treatment to high risk individuals who are acutely threatened by this disease process.
Researchers are also actively studying new treatments for geographic atrophy – including drugs that target the immune system and gene therapy. Additionally, low vision aids and assistive devices can help to improve the quality of life for people with GA by making it easier for them to perform daily tasks and activities.
Research is continually being conducted to combat Age-Related Macular Degeneration (AMD). Recent developments have offered hope in slowing the progression of AMD, as injectable medications and specially formulated over-the-counter vitamins can help preserve macular health.
For individuals with advanced age-related macular degeneration (AMD), accomplishing everyday tasks like reading the mail or interpreting a clock can be challenging. Fortunately, organizations exist to assist patients in selecting and obtaining helpful tools such as magnification devices, large print materials, and voice-activated watches that simplify daily living activities. These groups also provide resources regarding support groups and other accessible information concerning adaptive products, training programs for independent living skill sets, plus various types of assistive technologies – all designed to equip AMD sufferers with greater independence around their environment.
As you age, it is important to have regular visits with your eye doctor for screenings and examinations that may detect the early signs of AMD. Most people do not know that they have it until their vision has become blurry, and if left unchecked, the successful outcome of treatment decreases. AMD can be challenging, but with the help of the team at South Carolina Retina Institute, we aim to provide you with therapeutic treatment options to help prevent or slow down vision loss.